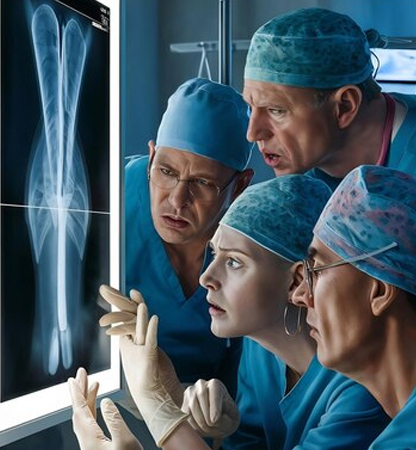
Orthopedic
Orthopedic practices face unique billing challenges due to the complexity of procedures, frequent use of imaging, and insurance nuances. Effective revenue cycle management (RCM) ensures smooth reimbursement and minimizes claim denials. Here’s how you can optimize your orthopedic medical billing process.
Common Challenges in Orthopedic Billing
1.Complex Coding for Procedures
- Orthopedic treatments involve multiple CPT codes, including surgical, non-surgical, and therapy-related codes.
- Incorrect coding can lead to claim denials or underpayment.
2.High Volume of Prior Authorizations
- Many orthopedic services, such as joint replacements and MRI scans, require prior authorization.
- Delays in obtaining authorization can result in claim denials.
3.Bundling & Unbundling Issues
- Some procedures are bundled under a single CPT code, and incorrect unbundling can lead to compliance issues.
4.Workers’ Compensation & Auto Accident Claims
- Handling third-party liability and understanding payer-specific rules is crucial for timely payments.
5.Frequent Denials & Appeals
- Claim denials often arise from missing documentation, incorrect modifiers, or lack of medical necessity.
- A structured appeal process helps recover lost revenue.
Best Practices for Optimized Orthopedic Billing
1. Accurate Documentation & Coding
- Ensure proper documentation of procedures, fractures, injections, and durable medical equipment (DME).
- Use appropriate ICD-10, CPT, and HCPCS codes to reflect medical necessity.
- Regularly train your billing team on orthopedic coding updates.
2. Streamline Prior Authorizations
- Maintain a checklist of procedures requiring prior authorization.
- Automate authorization tracking to prevent delays and rejections.
3. Use Correct Modifiers
- Apply Modifier 59 for distinct procedural services.
- Utilize Modifier 25 for evaluation and management (E/M) services performed on the same day as a procedure.
- Use Modifier 50 for bilateral procedures.
4. Optimize Claims Submission & Follow-Ups
- Ensure clean claim submission by verifying patient demographics, insurance details, and medical necessity.
- Regularly audit claims to reduce denials and resubmissions.
- Monitor reimbursement trends to detect payer-specific patterns.
5. Manage Workers’ Compensation & Liability Claims Efficiently
- Familiarize yourself with state-specific workers’ compensation guidelines.
- Follow up diligently on accident-related claims, as they often involve third-party payers.
6. Stay Updated with Insurance & Compliance Changes
- Medicare and private payers frequently update billing rules; staying compliant prevents penalties.
- Adhere to HIPAA regulations and maintain accurate patient records.


How Malakos Healthcare Solutions Can Help
At Malakos Healthcare Solutions, we specialize in orthopedic medical billing to ensure maximum reimbursements with minimal claim denials. Our expert team handles coding, prior authorizations, claims follow-ups, and appeals—so you can focus on patient care.


